Category: Nachrichten und interessante Infos
Verbreitung der LS bei Kindern:
- 1:5000 Kinder, damit also relativ häufig
Auslöser:
- Autoimmunerkrankung, keine Auslöser bekannt, in den meisten Fällen keine direkte Vererbung, jedoch eine Neigung zu Autoimmunerkrankungen kann vererbt werden
Wie erkennt man diese Erkrankung?
- Typische Hautveränderung entweder rundlich (Morphea), häufig auch lineare Hautveränderungen (lineare Sklerodermie), teilweise tiefe Sklerodermie (auf der Haut kaum sichtbar), aber unter der Haut eine Verhärtung tastbar, aber auch Mischformen
- Blaue Verfärbung bedeutet, dass Unterhautfettgewebe weniger geworden ist, gegangen ist, und weniger Fettisolierungsschicht vorhanden ist.
- Rötliche Verfärbung deutet auf eine vermehrte Durchblutung
Alle Körperteile können betroffen sein.
- Bei allen gelenksüberschreitenden Veränderungen und Veränderungen die zu
kosmetischen Problemen führen sollte eine systemische immunomodulierende Therapie
angefangen werden - Bei Beteiligung im Gesicht (Therapie möglichst frühzeitig mit autologen Eigen-Fettzell-
TPL, um Gewebe aufzufüllen. Möglich, dass dies mehrfach wiederholt werden muss.
Fettzellen werden im Oberschenkel abgesaugt. Narbengewebe kann dadurch
aufgeweicht werden)
a. Coup de Sabre (Cave! neurologische Beteiligung im Zentralnervensystem)
Häufige extrakutane Beteiligung (nicht nur die Haut betreffende Beteiligung):
- Gelenke (Arthritis) und Sehnenansätze (Enthesitis), auch in den Bereichen, wo
keine Hautbeteiligung ist) um 70% - Muskelschwäche durch Kontrakturen
- Verminderte Wachstum der betroffenen Extremität
- Auge- Regenbogenhautentzündung (um 1-5%)
- neurologische Beteiligung im Zentralnervensystem
- LS ist heimtückisch, schmerzt nicht, macht Kontrakturen (Bein-, bzw. Armlängendifferenz)
Darum frühzeitige Therapie, verkürzte Extremitäten wachsen nicht nach und unbehandelt kann
es zu schweren Veränderungen kommen - Suizid bei Kindern mit LS im Gesicht hoch, darum möglichst rechtzeitig Therapie einleiten
- 70% Gelenkbeteiligung davon 50% nicht an der Stelle der betroffenen Haut!! Bei Erkrankung
im Gesicht auch immer Kiefergelenke untersuchen lassen)
Gibt es Schübe?
- Ja. Deswegen sollte der Arzt immer auch alle Körpersetellen nach neuen Hautveränderungen
und die Gelenke am ganzen Körper anschauen und die Patienten sollten immer vom Kinder-
(Erwachsehenen-Rheumatologen und Dermatologen betreut werden (siehe aktuelle Leitlinie) - Regelmäßige Uveitis Screenings
Sind Kinder und Erwachsene als Patienten vergleichbar?
- Ja, es gibt einen identischen Verlauf und eine identische Therapie
Ist LS vererbbar?
- Nachkommen haben die „Disposition“ eine Autoimmunerkrankung zu bekommen. Keine 1:1
Vererbung.
Ist LS heilbar?
- Nein, aber es ist sehr gut kontrollierbar, bei rechtzeitiger effektiver Behandlung kommt es zu
Inaktivität. Nach 2-3 Jahren Inaktivität, kann man versuchen die Medikation abzusetzen und es
kann auch eine Ruhephase ohne Medikation geben. In dieser Zeit trotzdem immer zu den
Kontrollen sinnvoll.
Behandlung(1): alle Medikamente sind off label
- Methotrexat (15mg/m²/Woche) oral oder subkutan
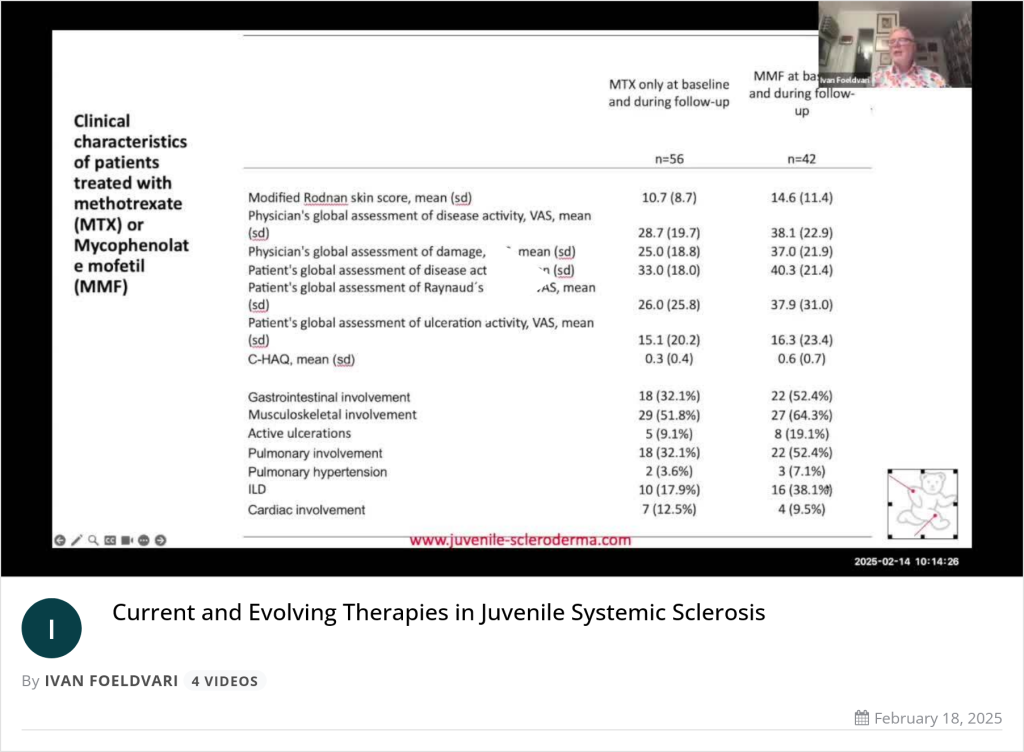
Bei Unverträglichkeit von Methotrexat ist Mycophenolat eine Option (1200 mg/m2/Tag) //
alternativ Mycophenolat Mofetil (MMF) 1200 -1500 mg /m2/Tag oral - Eskalieren der Therapie nach nichtansprechen auf Methotrexat nach 3-4 Monaten mit
Abatacept (Abatacept – Anwendung, Wirkung, Nebenwirkungen | Gelbe Liste (gelbe-
liste.de) oder Toxilizumab RoActemra® Fertigspritze (fachinfo.de)-.beide Therapien sind
off Label, sie müssen beantragt werden - Evtl. JAK-Inhibitoren ( off label)
Referenzen
- Foeldvari I, Marrani E. Systemic therapy in juvenile localized scleroderma. Expert Rev
Clin Immunol. 2023;19(10):1225-38. - Marrani E, Foeldvari I, Lopez JA, Cimaz R, Simonini G. Comparing ultraviolet light A
photo(chemo)therapy with Methotrexate protocol in childhood localized scleroderma: Evidence
from systematic review and meta-analysis approach. Semin Arthritis Rheum. 2018;48(3):495-
503. - Constantin T, Foeldvari I, Pain CE, Palinkas A, Hoger P, Moll M, et al. Development of
minimum standards of care for juvenile localized scleroderma. Eur J Pediatr. 2018;177(7):961-
77.
Nebenwirkungen:
- Übelkeit, dann kann ggf. auf MMF umgestellt werden (es ist ein off Label Therapie muss beantragt werden)
- Keine der Therapien hat Einfluss auf Fertilität
- Bei allen erwähnten Therapien wird eine Verhütung empfohlen
Gibt es alternative Behandlungsansätze:
- Lichttherapie ist ineffektiver als MTX(2), unter 12 Jahren nicht empfohlen (Risiko für Hautkrebs)
für Weiteres Keine Datenlage, nicht evidenzbasiert - Bei Patienten , wo die Läsionen die Gelenke betreffen und mögliche kosmetische Schänden
auftreten, wird kein Lichttherapie empfohlen (3)
Bis wann können Kinder zum Pädiater gehen:
- Bis 18-21 Jahren, dann Transition in der Erwachsenen Rheumatologie
Gibt es Besonderheiten, die beim Sport oder in der Schule zu beachten sind:
- Nein, Sport ist gut und wird empfohlen
Gibt es Ernährungstipps:
- Nein keine Empfehlung, gesunde Mischkost
Impfempfehlungen:
- Nach STIKO ohne Medikation
- Unter den empfohlenen Medikationen nur inaktive Impfungen, kein Lebendimpfstoff
(Mumps, Masern, Röteln)
Bei Fragen:
Dr. Ivan Foeldvari – www.kinderrheumatologie.de
Category: Nachrichten und interessante Infos
Dr. Ivan Foeldvari wurde eingeladen, am 19.11.2024 auf dem Rheumakongrerss November 2024 in Wahington, DC, USA, einen Übersichtsvortrag über die Therapie der juvenillen sysemischen Sklerodermie zu halten.
Category: Nachrichten und interessante Infos
Dr. med. Stefanie Tatsis und Dr. med. Ivan Foeldvari erörtern die Herausforderungen und neuesten Erkenntnisse zur Transition in der rheumatologischen Versorgung, insbesondere den Übergang von der pädiatrischen zur erwachsenen Rheumatologie. Sie erläutern, wie eine altersgerechte Betreuung gewährleistet werden kann und welche Strategien für eine erfolgreiche Transition von entscheidender Bedeutung sind. Schauen Sie gerne rein!
Link zum Video für Fachpublikum (Login über DocCheck notwendig)
Category: Nachrichten und interessante Infos
Congratulations to: Ivan Foeldvari
whose paper has been recognized as a top cited paper* in:
ARTHRITIS CARE & RESEARCH
New and Updated Recommendations for the Treatment of Juvenile Idiopathic Arthritis-Associated Uveitis and Idiopathic Chronic Anterior Uveitis
*Among work published between 1 January 2022 – 31 December 2023.
Category: Nachrichten und interessante Infos
Rheuma? Das ist doch eine Erkrankung, die ältere Menschen plagt – so denken viele.
Dr. Ivan Foeldvari, Hamburger Zentrum für Kinder- und Jugendrheumatologie, berichtet im Hamburger Ärztemagazin Dezember 2023.
Externer Link zum Beitrag: Auch Kinder können Rheuma haben (PDF)
Category: Nachrichten und interessante Infos
The result of the International Hamburg Consensus Meeting December 2022
More information:
https://www.tandfonline.com/doi/full/10.1080/1744666X.2023.2298354
Category: Nachrichten und interessante Infos